The facility-wide surveillance program is a continuous process of systematic collection, consolidation, and analysis of data concerning the distribution and transmission of infections within an identified population. Device-associated infections and infections with high morbidity and mortality should be assessed for a root cause. Facility-wide targeted surveillance is the primary focus. The categories included in the targeted surveillance groups are those that present the greatest potential for harm and liability and are typically the most common or have epidemiological significance. Surveillance information is disseminated to those who can reduce the incidence and improve outcomes including leadership, clinical staff, providers, residents and families. McGeer’s and the National Healthcare Safety Network (NHSN) criteria should be used for surveillance definitions.
The Infection Preventionist monitors for:
- Catheter-associated central line infections (CLABSI)
- Catheter-associated urinary tract infections (CAUTI)
- Clostridioides difficile (CDI) infections
- Communicable disease transmission
- Gastrointestinal (GI) infections
- Multidrug-resistant organisms (MDRO)
- Respiratory infections
- Urinary tract infections (UTIs)
- Sepsis
Journal Article
Sample McGeer's Criteria - Revised McGeer Criteria for Infection Surveillance Checklist >
National Healthcare and Safety Network (NHSN) Resources:
-
Surveillance Definitions
-
Date of Event (DOE): The date the first element used to meet the criteria for site-specific infections occurs for the first time within the seven-day infection window period.
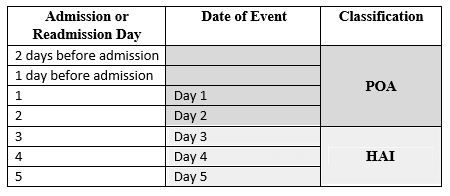
Healthcare-associated Infection (HAI): Is the date of event of the site-specific infection criterion that occurs on or after the 3rd calendar day of admission or readmission, where day of admission is calendar day 1.
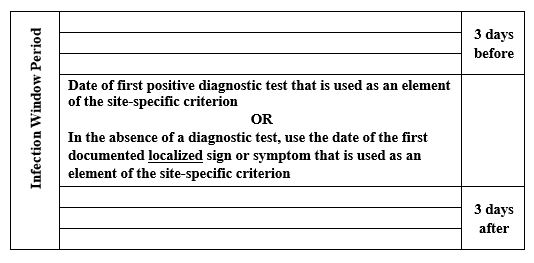
Infection Window Period (IWP): Is defined as the 7-days during which all site-specific infection criteria must be met. It includes the collection date of the first positive diagnostic test that is used as an element to meet the site-specific infection criterion, the 3 calendar days before and the 3 calendar days after.
Examples of diagnostic tests:
- laboratory specimen collection
- imaging test
- procedure or exam
- physician diagnosis
- initiation of treatment
For site-specific infection criteria that do not include a diagnostic test, the date of the first documented localized sign or symptom that is used as an element of the site-specific infection criterion is used to define the infection window period (IWP), for example, diarrhea, site-specific pain, or purulent drainage.
Present on Admission (POA): Is the day of admission or readmission to an inpatient location (calendar day 1), the 2 days before admission or readmission, and the calendar day after admission or readmission.
Repeat Infection Timeframe (RIT): Is a 14-day timeframe during which no new infections of the same type are reported. The Date of Event (DOE) is Day 1 of the 14-day RIT.
Secondary Bloodstream Infection Attribution Period (SBAP): Is the period in which a blood specimen must be collected for a secondary bloodstream infection to be attributed to a primary site infection. This period includes the Infection Window Period (IWP) combined with the Repeat Infection Timeframe (RIT). The SBAP is 14-17 days in length depending upon the Date of Event.
To determine if an infection is healthcare-associated, the first step is to determine when the infection started. The first element of the site-specific criteria needs to be determined, which is the date of event (DOE), in the infection window period (IWP). If the first element was on the day of admission or readmission (calendar day 1), the 2 days before admission or readmission, or the calendar day after admission or readmission the infection is POA and not healthcare-associated.
Infection Window Period (IWP)
Date of Event and Classification Determination:
A site-specific infection should only be counted once in a 14 day period. If criteria for the same type of infection are met and the Date of Event (DOE) is within the 14-day RIT period, the new event is not identified or reported and is a continuation of the last infection. Additional pathogens recovered during the RIT from the same type of infection are added to the original event and not counted again.
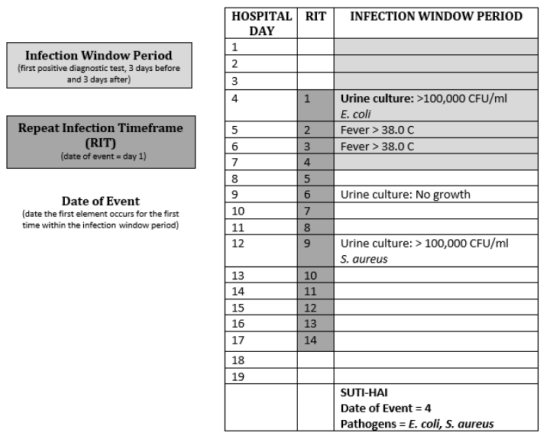
*The National Healthcare Safety Network (NHSN) has worksheet generators to help determine DOE, IPW, RIT and secondary bloodstream infections >
-
Communicable Diseases and Reportable Infections
-
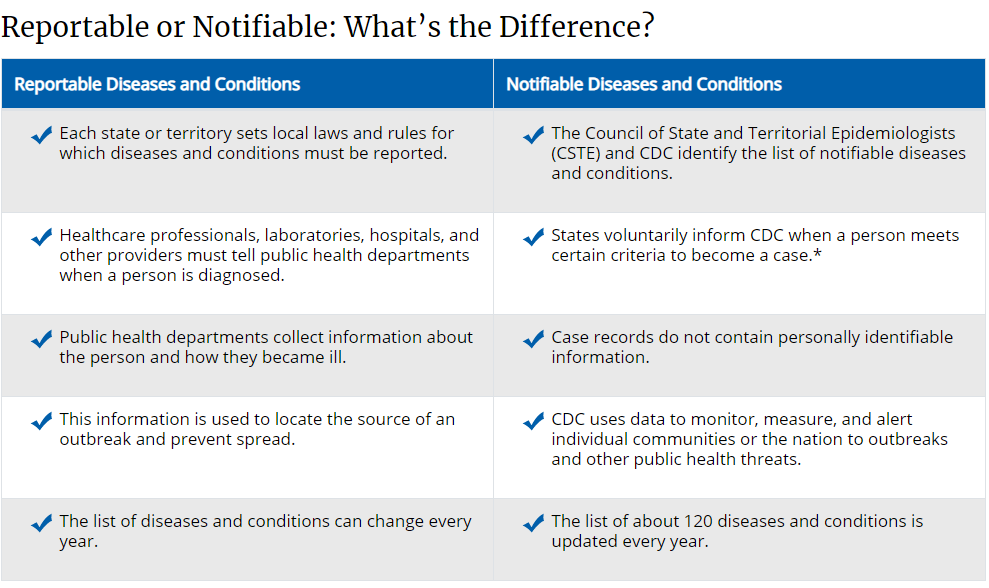
Case surveillance starts at the local level; it’s the foundation of public health practice and is used to understand how diseases spread with the goal of preventing future transmission. Local laws and regulations determine which diseases and conditions are reportable. The Infection Preventionist should be familiar with disease reporting in the state of N.J. Discuss reporting results with the lab that is used for testing. Some reportable organisms are automatically reported. Contact the Department of Health if there are questions.
- How to report in New Jersey >
- Tips of Communicable Disease Reporting >
- New Jersey Reportable Diseases >
- CDC National Notifiable Diseases Surveillance System (NNDSS) >
The National Notifiable Diseases Surveillance System (NNDSS) is used by the CDC to gather data on diseases from 3,000 health departments throughout the U.S. NNDSS uses disease data to recognize outbreaks, track spread, identify areas of concern, identify groups most at risk and evaluate control activities.
-
Outbreak Identification
-
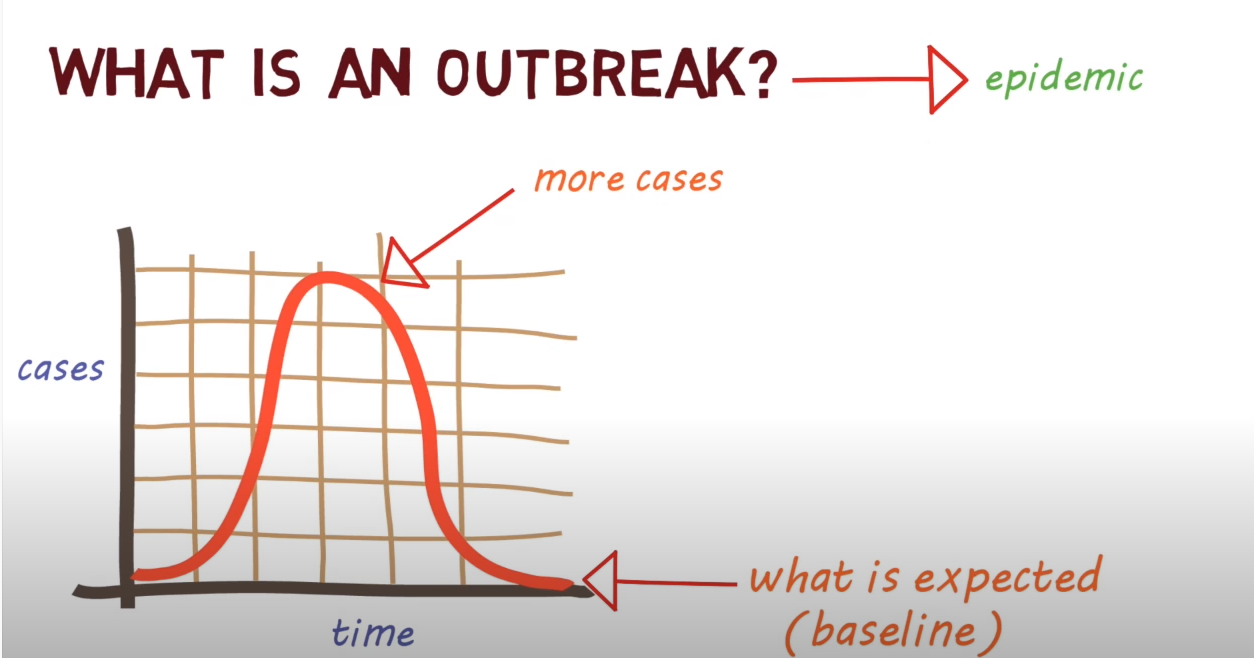
An outbreak is the occurrence of more cases of a disease or infections than would normally be expected in a specific place or group of people over a given period, per the Centers of Disease Control and Prevention. Outbreaks and clusters are reportable events. Contact your local health department for more details.
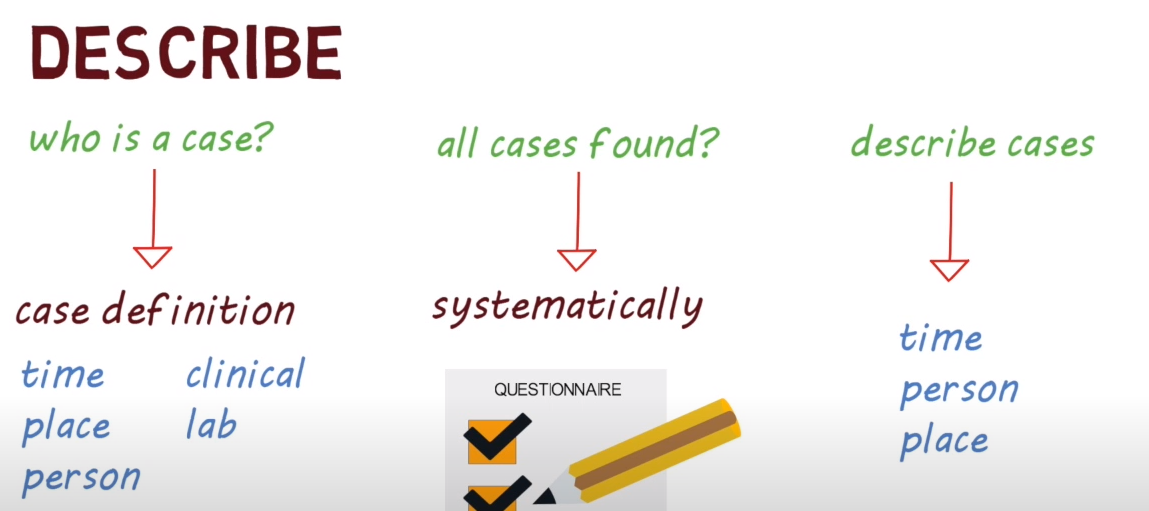
A clear case definition is critical to effectively investigating an outbreak. The use of common case definitions allows for standardization of the cases within an ongoing outbreak investigation and possibly between outbreak investigations that differ over time or geographic location. The facility’s local health department can help determine an outbreak definition.
General guidelines for outbreak case definitions: Criteria for person, place, time, and clinical features. These should be specific to the outbreak under investigation.
- "Person" describes key characteristics the residents or staff have in common. For example: age, sex, race, and exclusion criteria (e.g., “persons with no history of X disease”)
- "Place" typically describes a specific geographic location within the facility associated with the outbreak (X unit, Y activity)
- "Time" is used to delineate the period associated with illness onset for the cases under investigation. Limiting the time period allows for exclusion of similar illnesses which are unrelated to the outbreak of interest
- “Clinical features" should be simple and objective (e.g., sudden onset of fever and cough, or laboratory findings)
Once a case definition is determined, individuals meeting the criteria will be included in an outbreak investigation.
- All outbreak investigations should be immediately reported to the administrator, the medical director, clinical leadership, and the local department of public health for prevention measures and assistance with the investigation.
Goal: promptly identify problematic pathogens, stop ongoing disease transmission, and reduce risks for future events.
- Disease outbreaks are adverse events which can occur in any health care setting and pose a threat to patient safety and lives.
- Investigation of a potential outbreak involves certain predictable epidemiological elements.
Key Terms
- Cluster: is an aggregation of cases grouped in place and time that are suspected to be greater than the number expected, even though the expected number may not be known.
- Outbreak: an increase in the occurrence of cases of infection or disease over what is expected in a defined setting or group in a specified time period; synonym of epidemic but used more often when limiting the geographic area.
- Endemic: is the constant presence/ usual level, or prevalence, of a disease or infectious agent in a population within a geographic area.
- Epidemic: is an increase over the endemic level of a disease, often sudden, in a population or region over a particular period of time.
- Pandemic: is an epidemic that has spread over several countries or continents, usually affecting a large number of people.
- Line list: a list established to assist and guide an outbreak investigation by documenting and organizing demographic data, clinical risk factors, and host or other contributing factors.
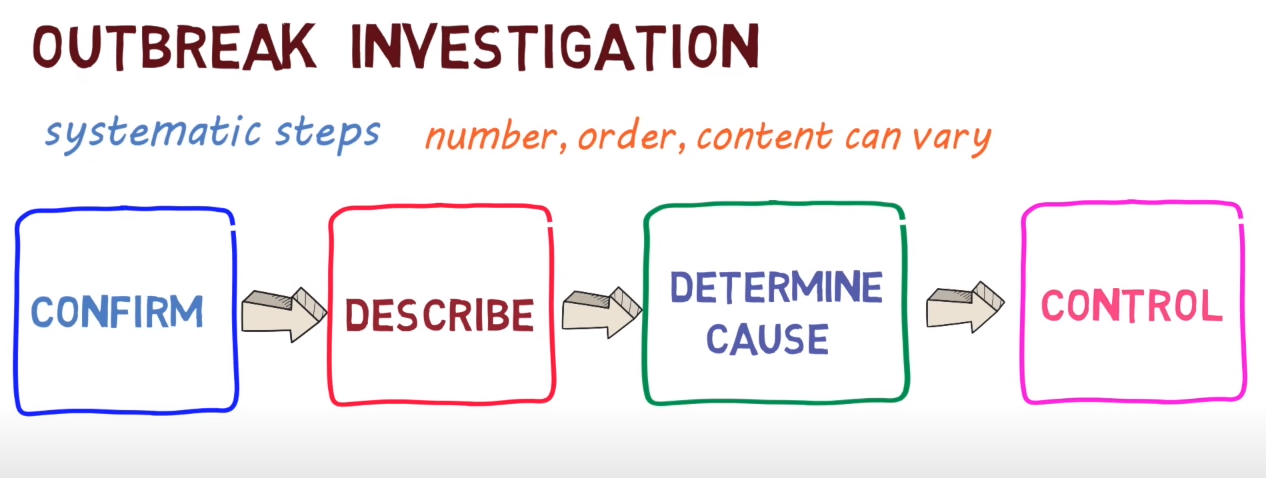
Investigations of outbreaks are required to be conducted in a standardized way.
Areas that must be assessed include:
- The agent (virus, bacterium, parasite, or another microbe)
- The host (refers to humans that get the disease)
- The environment (refers to extrinsic factors that affect the agent and opportunity for exposure).
The goal of any outbreak investigation is to control the outbreak by identifying and modifying contributing factors and to develop and implement measures to prevent similar outbreaks in the future.
Investigation Components
The CDC’s primary components of the initial investigation include:
- Confirming the presence of an outbreak
- Identifying investigation team and resources
- Verifying the diagnosis
- Establishing a preliminary case definition
- Alerting administration and key health care partners about the investigation
- Performing a detailed literature review
- Developing a methodology for case findings
- Preparing an initial line list and contact trace
- Observing and reviewing potentially implicated care activities
- Considering whether environmental sampling or HCP sampling should be performed
- Implementing initial control measures
- Defining and refining the case definition
- Continuing case findings and surveillance
- Reviewing regularly control measures
- Maintaining surveillance activities
- Considering whether an analytic study should be performed.
Confirming Presence of an Outbreak
- When a possible outbreak is reported, the initial step in the investigation is to confirm and validate the information.
- Is there an increase over baseline? Compare normal levels? Surveillance data?
- Are there other causes? Increased testing, lab error, increase in population??
- IMMEDIATE CONTROL.
Identifying Investigation Team and Resources
- Get an investigation team together- the size depends on the nature of outbreak.
Verifying the Diagnosis: Clinical Findings and Lab Data
- Verification of the clinical and laboratory diagnosis is vital in an investigation.
Establishing a Preliminary Case Definition
- The initial case definition should be narrow enough to focus investigative efforts but broad enough to capture the majority of cases.
- Outbreaks of infections with careful consideration should be given to whether the case definition should have a microbiologic component.
- Requiring that cases have a culture for a specific organism is both focusing the investigation and facilitating case findings. However, in some instances, this requirement might also miss cases. (For example, influenza-like illness might be preferred to confirmed influenza with review of the clinical symptoms).
Developing a Methodology for Case Findings
- Variety of sources to find additional cases that might be related to the outbreak: Lab data, signs and symptoms.
- Point prevalence to determine colonization or infection rates.
Alerting Administration and Key Health Care Partners about the Investigation
- At the outset of an outbreak investigation, it is critical to inform key partners of the expanding situation. Federal and state agencies have specific reporting requirements that are often time sensitive.
Performing a Detailed Literature Review
- There are many reports summarizing outbreak investigations published in the literature, and hence a literature review is a critical early step in any investigation. The literature review will help identify possible sources which merit further investigation and might also provide important insight into optimal investigative methodology.
- CDC, AJIC, National Library of Medicine, communicable disease manuals.
Preparing an Initial Line List and Contact Trace
- The line list is perhaps the single most important tool in any outbreak investigation
- Developing them is a resource-intensive activity because it involves a review of a variety of different sources of information: medical records, patient locations and movement, staff interviews. Each ill resident or staff member information is entered in a unique row on the line list. Line lists should be updated and reviewed daily.
- Contact tracing is the identification and diagnosis of people who may have come into contact with an infected person. How to conduct a contact trace will depend on the diseases.
- It is critical to carefully weigh the benefits of any information to be included on the line list against the resources required to obtain it.
- Customizable line list templates that may be used to collect basic information upon notification of a potential outbreak or cluster are readily available on many public health websites.
Implementing Infection Prevention and Control Measures Throughout the Course of the Investigation
- Isolate
- Cohort
- Modify/Increase Cleaning
- Audit practices with real-time coaching
- Exclude ill staff from work
- Education and in-services for health care team.
Observing and Reviewing Potentially Implicated Care Activities
- Observations of clinical practices may ultimately identify the cause
- Line list is critical in helping guide both the type and location of observations that will need to be done
- Pay careful attention to how practices might differ among health care workers
- Observations should also review adherence to general infection prevention practices (teachable moments).
Documenting Communication and Lessons Learned
Communication During and After an Outbreak Investigation
- Public Health, Administration, clinicians, residents, other health care workers (case by case)
- Communicate with other facilities before transport using universal transfer sheet.
More Information