- Aspergillus
- - a type of fungus that people breath in every day. People effected by Aspergillus infections are people with weak immune systems and lung disease. Healthcare-associated invasive infections are associated with building renovations and construction due to dust exposures. Outbreaks of cutaneous infections have been linked to contaminated biomedical devices.
- Bedbugs
- - parasitic as they feed on human blood, but they do not live on people. They come out at night to feed, living in the environment, usually cracks and crevices of beds, box springs, headboards, ceilings and walls.
- Burkholderia cepacian
- - a gram-negative bacteria found in the environment including water and soil that cause little risk to healthy people by has cause significant outbreaks in healthcare settings including contamination of prefilled saline syringes and liquid docusate.
- Candida auris
- - a fungus that is an emerging global health threat. This organism is multidrug-resistant, difficult to identify in standard labs and has caused outbreaks in the healthcare setting. Approximately 30-60% of people infected will die from this organism.
- Carbapenem-resistant Enterobacterales (CRE)
- - a group of drug-resistant bacteria found in the human intestines. These organisms can be found in skins and drains. According to the CDC, CRE are a serious threat to public health and are associated with mortality rates of up to 50% for hospitalized patients. Due to the movement of patients throughout the health care system, if CRE are a problem in one facility, then typically they are a problem in other facilities in the region as well, the agency said.
- Clostridioides difficile (C. diff or CDI)
- - a type of gram-positive spore forming bacteria that produces and endotoxin (either A or B) commonly found in the large intestine.
- ESBL-producing Enterobacterales
- - a large order of many different types of bacteria that produce an enzyme that breaks down antibiotics making the antibiotic ineffective. There organisms are usually found in the human intestines, but food and water contamination are unclear. This order includes E. coli and K. Pneumonia.
- Viral Hepatitis
- - a group of viruses known to cause liver disease although rare with Hepatitis A. Hepatitis A is spread through the oral-fecal route. Hepatitis B & C are bloodborne pathogens. There is also Hepatitis D & E. Hepatitis D only occurs with a hepatitis B infections as this virus is a “delta hepatitis”. Hepatitis D needs the B virus to cause infections. Hepatitis E in the US is usually from raw or undercooked pork, venison or shellfish.
- HIV/AIDS
- Human immunodeficiency virus (HIV) is a bloodborne pathogen that can lead to acquired immune deficiency syndrome (AIDS). It’s is rarely spread in healthcare. Once individuals are infected this makes them venerable for other types of infections.
- Influenza
- - a virus that is classified by subtypes of surface proteins of H (hemagglutinin) and N (neuraminidase). Different species can carry influenza including birds, pigs and dogs. Influenzas rarely cross species to humans (antigenic shift). When they do it usually results in a pandemic.
- Klebsiella pneumoniae
- - a gram-negative bacteria commonly found in the human intestines. This organism can become a CRE and is known to cause healthcare-associated infections and outbreaks.
- Legionellosis
- - a gram-negative bacteria that was discovered in the Philadelphia, Pennsylvania in 1976 at an American Legion’s convention. It’s found in water and infects the lungs.
- Lice
- - parasites that can live in hair, eyebrows, eyelashes, beards, on the chest and armpits. There are three types: head lice (Pediculus humanus capitis), body lice (Pediculus humanus corporis) and pubic lice (Pthirus pubis).
- Methicillin-resistant Staphylococcus aureus (MRSA)
- - a type of drug-resistant bacteria that lives on people’s skin. Around 33% of people carry Staphylococcus aureus on their skin and two people out of one hundred carry the drug-resistant strain. With about five percent of hospitalized patients having MRSA in their nose or on their skin. MRSA infections are still a serious health threat. Staphylococcus aureus can also become vancomycin-resistant.
- Tuberculosis (TB)
- - caused by a slow growing bacteria that usually infects the lungs, but it can also be found in other parts of the body like the kidneys, spine and brain. TB outside of the lungs is extrapulmonary TB; it’s rarely contagious.
- Norovirus
- - a virus that is commonly found in the gastrointestinal tract, food and water. It is the leading cause of contaminated food outbreaks in the Unites States.
- Pseudomonas aeruginosa
- - a gram-negative bacteria commonly found in the environment including water and soil. Individual who are on ventilators, have catheters and wounds are at increased risk.
- Scabies
- - parasites that live on the human body. First time infection symptom do not appear for 2-6 weeks. If a person has had scabies in the past symptoms start in 1-4 days. Crusted or Norwegian scabies are of very sever contagious form of scabies and occur in people that are immunocompromised including the elderly.
- Vancomycin-resistant Enterococcus (VRE)
- - a group of bacteria that are drug-resistant. There are often found in human intestines, female genitals, soil and water.
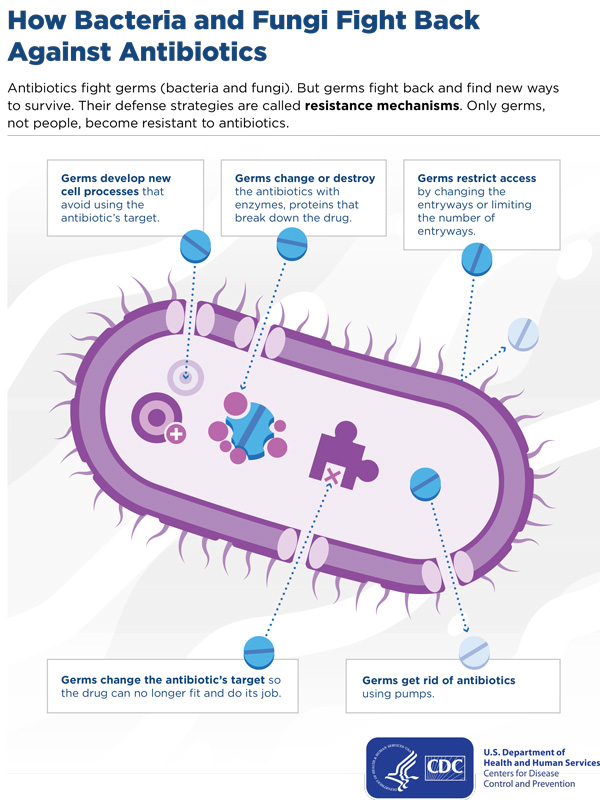
Multidrug-Resistant Organism
Penicillin was discovered in 1928 by Alexander Fleming. The first drug-resistant organism was identified in 1942. Antibiotic resistance occurs when an organism develops a way to defeat the antibiotics designed to kill them. This can happen several different ways. Microorganisms can restrict the entryway or limit the number of entryways so an antibiotic cannot get in. Microorganisms can produce a pump to get rid of an antibiotic that enters and push it back out. A microorganism can change the antibiotics target making it useless or they can develop a way to change the antibiotic target, again making it useless. Or microorganisms can produce enzymes that can destroy the antibiotics completely, which is how ESBLs become resistant. Other organisms, like a certain group of CREs called CP-CREs (Carbapenemase Producing Carbapenem-Resistant Enterobacteriaceae), can share their genetic resistance with other non-resistant bacteria causing more drug-resistant organisms. As new antibiotics are developed microorganisms find a way to survive. Colistin is used as a last-line treatment for Carbapenem-resistant Acinetobacter baumannii (CRAB), some of these organisms have become resistant to colistin.
In 2019 the CDC published Antibiotic Resistance Threats in the United States. There are more than 2.8 million drug-resistant infections that occur each year with more than 35,000 deaths. Any organism can become drug-resistant including influenza. There are many different types of bacteria and fungus listed in the report (see below) that the CDC has placed into three categories of concern. There are some organisms that have become pan-resistant, which means the organisms are resistant to all antibiotics that are used to treat them and there are no treatment options left.
CDC Urgent Threats:
- Carbapenem-resistant Acinetobacter
- Drug-resistant Candida auris
- Clostridioides difficile (C. difficile)
- Carbapenem-resistant Enterobacteriaceae
- Drug-resistant Neisseria gonorrhoeae
CDC Serious Threats:
- Drug-resistant Campylobacter
- Drug-resistant Candida species
- Extended-Spectrum Beta-Lactamase Producing Enterobacteriaceae (ESBL)
- Vancomycin-resistant Enterococci (VRE)
- Multidrug-resistant Pseudomonas aeruginosa
- Drug-resistant nontyphoidal Salmonella
- Drug-resistant Salmonella serotype Typhi
- Drug-resistant Shigella
- Methicillin-resistant Staphylococcus aureus (MRSA)
- Drug-resistant Streptococcus pneumoniae
- Drug-resistant Tuberculosis (TB)
CDC Concerning Threats
- Erythromycin-resistant Group A Streptococcus
- Clindamycin-resistant Group B Streptococcus
CDC Watch List
- Azole-resistant Aspergillus
- Drug-resistant Mycoplasma genitalium
- Drug-resistant Pertussis (Whooping Cough)
The New Jersey Department of Health requires health care facilities to report MDROs when transporting patients and residents between facilities. This should be done both verbally and written prior to transfer.
Epidemiological significant organism seen in health care of concern for outbreaks in the long-term care setting are multidrug-resistant Candida auris, carbapenem-resistant Acinetobacter baumannii (CRAB) and Carbapenemase Producing Carbapenem-Resistant Enterobacteriaceae (CP-CRE). Prevention measures for these organisms are early detection, prompt isolation and communication between health care facilities. The CDC recommends either Contact Precautions or Enhanced Barrier Precautions for any individual colonized or infected with these organisms. Individuals can have active infections or colonization of any of these organisms.
-
Candida auris
-
Candida auris is considered a serious global health threat by the CDC. C. auris is a fungus that is spread from person to person or through contaminated surfaces and equipment. C. auris does not respond to many antifungal medications requiring higher doses and multiple classes of antifungals. This organism causes bloodstream infections, wound infections and ear infections. Nursing home patients and residents are at higher risk for transmission. The CDC has been tracking C. auris in the U.S. since 2013.
Infection prevention and control recommendations for Candida auris in skilled nursing and subacute rehabilitation facilities
Nursing home residents should be placed on Enhanced Barrier Precautions during high-contact activities which include the use of gowns and gloves during the following activities:
- Dressing or Bathing/showering
- Transferring
- Providing hygiene
- Changing linens
- Changing briefs or assisting with toileting
- Device care or use: central line, urinary catheter, feeding tube, tracheostomy/ventilator
- Wound care: any skin opening requiring a dressing.
Nursing home residents on Enhanced Barrier Precautions can leave their rooms as long as secretions, excretions, and bodily fluids are contained and the resident can perform hand hygiene when appropriate (e.g., prior to leaving their room).
Contact Precautions should be used for residents with acute diarrhea, draining wounds, or other sites of secretions or excretions that are unable to be covered or contained.
Environmental cleaning and disinfection should be done with an EPA-registered hospital grade disinfectant for C. auris which can be found on the EPA’s List K (EPA’s Registered Antimicrobial Products Effective Against Clostridium difficile Spores).
Rehabilitation and Shared Services:
- Staff providing therapy to residents with C. auris should not work simultaneously with other residents
- Whenever possible, schedule resident with C. auris for therapy services at the end of any given day
- Shared equipment should be thoroughly cleaned and disinfected after use, as described above.
-
Carbapenem-resistant Acinetobacter baumannii (CRAB)
-
Carbapenem-resistant Acinetobacter baumannii (CRAB) causes infections in the blood, urinary tract, lungs and wounds. CRABs are resistant to many antibiotics including carbapenems. Carbapenems are usually the last line of defense for MDROs. Infections usually occur in the health care settings and outbreaks are seen in many long-term care facilities. The rate of mortality is high. This organism is spread through contaminated environmental surfaces and shared equipment or from person-to-person. This organism is also tracked by the CDC. Enhanced Barrier Precautions and Contact Precautions should be used for these organisms as outlined C. auris.
-
Carbapenemase Producing Carbapenem-Resistant Enterobacteriaceae (CP-CRE)
-
Carbapenemase Producing Carbapenem-Resistant Enterobacteriaceae (CP-CRE) CREs are a group of microorganisms (Enterobacteriaceae) that are resistant to a group of antibiotics (Carbapenemase). CP-CRE are a subset of all CREs. They that produce carbapenemase which is an enzyme that breaks down the carbapenem antibiotics making them ineffective. Enterobacteriaceae that can become CP-CREs are E. coli, Klebsiella spp., or Enterobacter spp. Enhanced Barrier Precautions and Contact Precautions should be used for these organisms as outlined for C. auris.
Clostridioides difficile and other Diarrheal Illnesses
Clostridioides difficile formally known as Clostridium difficile is a spore producing bacteria that causes diarrhea and colitis. One in eleven individuals over the age of 65 will die within one month of diagnosis of a health care-associated infection, while another one in six patients will get C. diff again within two to eight weeks. C. diff is considered an urgent threat by the CDC. In 2017 there was approximately 223, 900 hospitalized patients with C. diff and 12,800 deaths. C. diff can easily spread from person-to-person in a health care setting. C. diff infection risk factors include antibiotic use.
Prevention measures in a health care setting including long-term care:
- Use antibiotics appropriately
- Use Contact Precautions for residents with known or suspected cases to include the use of gowns and gloves. Using gloves to prevent hand contamination is key for preventing C. diff transmission via the hands
- Use of soap and water to clean hands after contact as it is more effective than alcohol-based hand rubs. However, early experimental data suggest that, even using soap and water, the removal of C. diff spores is more challenging than the removal or inactivation of other common pathogens. Friction is important for removal of spores
- Dedicate medical equipment to the resident whenever possible
- Continue these precautions until diarrhea ceases for 24 hours. Individuals can continue to shed the organism for several days following diarrhea, therefore some institutions routinely continue isolation several days beyond symptom resolution.
- Implement an environmental cleaning and disinfection program to include:
- Environmental surfaces and reusable devices likely to be contaminated with feces and surfaces that are touched frequently are cleaned often
- Daily room cleaning
- Terminal room cleaning when diarrhea has ended
- Use an EPA-registered disinfectant with a sporicidal claim for environmental surface and equipment listed on EPA List K that are registered as effective against C. diff spores
- Follow the manufacturer’s instructions for use (IFUs) for disinfection.
Individuals with diarrhea should be treated as infectious and follow the same precautions as noted for C. diff until an infectious process can be ruled out.
Other infectious diarrheal agents include:
Parasites: Lice and Scabies
Lice and scabies are parasitic insects that can be found on individuals and are easily spread by close person-to-person contact. Only body lice are known for transmitting diseases. Lice and scabies move by crawling. They do not hop, jump or fly. Dogs, cats and other animals do not transmit human lice and scabies.
Pediculus humanus capitis are head louse; adults are between 2.1 and 3.3 mm. They usually infest the head and neck area attaching their eggs to the hair shafts.
Pediculus humanus corporis are body lice; adults are between 2.3-3.6 mm. They lay their eggs and live on clothing but feed on skin.
Pthirus pubis are pubic lice. They are 1.1 to 1.8 mm and can live in course hair anywhere on the body including eyelashes, beards and armpits.
Sarcoptes scabiei var. hominis are human scabies that are an itch mite who lives and lays eggs in the upper layer of the skin causing a pimple-like rash. Common sites for scabies include wrists, elbows, armpits, webbing between the fingers, nipples, penis, waist, beltline, and buttocks.
Norwegian (crusted) scabies is a severe form of scabies that occurs in the elderly and immunocompromised. The skin is crusted because of large numbers of mites and eggs. Crusted scabies should be treated quickly and aggressively to prevent outbreaks.
Strict Contact Precautions and treatment should be used with parasitic insects to prevent outbreaks in a facility.
Mycobacterium Tuberculosis
Mycobacterium tuberculosis (TB) should not be confused with other types of Mycobacterium like Mycobacterium leprae (leprosy) or Mycobacterium avium. TB is a microorganism that is spread from person-to-person through the air and usually effects the lungs. TB occurs in communal settings and is significant in long-term care facilities because it spreads quickly among immunocompromised individuals. Individuals can be infected with latent TB, which means they have the microorganism but are not sick or symptomatic. Latent TB is not contagious. Individuals with latent TB can develop the disease in the future. Individuals with active TB are sick and can spread the disease. Extrapulmonary TB is when the microorganism is outside the lungs. It can be found in the abdomen, bones, and kidneys. If extrapulmonary TB is discovered the resident should be tested for pulmonary disease.
TB in the lungs can cause:
- a bad cough that lasts longer than 2 weeks
- pain in the chest
- coughing up blood or sputum (phlegm from deep inside the lungs).
Other symptoms of pulmonary TB disease are:
- weakness or fatigue
- weight loss
- no appetite
- chills
- fever
- sweating at night.
Prevention of pulmonary TB transmission requires early detection, isolation and treatment. Both residents and health care workers need to be screened for TB. Health care workers need to be screened pre-placement, after an exposure and annually. Pre-placement and post-exposures require a TST (tuberculin skin test) or IGRA (Interferon-Gamma Release Assays) test. Annual screening of health care workers should be done with testing based on an individual’s risk for TB. Health care workers with a history of latent TB or TB should not be tested.
- Signs and symptoms check
- Chest x-ray
The following actions are mandatory under the New Jersey Public Employees Occupational Safety and Health TB Requirements:
- Develop a written protocol for the early identification of individuals with suspected or confirmed infectious TB
- Provide medical surveillance for employees (following the latest CDC Guidelines)
- Provide case management of infected employees (following the latest CDC Guidelines)
- Report cases of TB
- Provide employee education and training
- Implement engineering controls (when required)
- Provide employees with and ensure the use of respiratory protection (when required) in compliance with the PEOSH Respiratory Standard (29 CFR 1910.134).
Legionnaires’ Disease and Pontiac Fever
Legionella bacteria can cause a serious type of pneumonia called Legionnaires’ disease and a less serious illness called Pontiac fever. All health care facilities should have a water management plan to prevent Legionella infections.
Zoonotic Diseases
Animals in health care facilities could potentially transmit zoonotic organisms from animals to residents, visitors and employees. Dogs and cats are commonly encountered in long-term care settings. Other animals also can be present. These animals can serve as reservoirs for zoonotic pathogens that could potentially infect people. Animals can also serve as reservoirs for multidrug-resistant organisms.
CDC: Examples of diseases associated with zoonotic transmission >
Virus
| Infectious Disease | Cats | Dogs | Fish | Birds | Rabbits | Reptiles | Primates | Rodents |
|---|---|---|---|---|---|---|---|---|
| Lymphocytic choriomeningitis | X | |||||||
| Rabies | X | X |
Bacteria
| Infectious Disease | Cats | Dogs | Fish | Birds | Rabbits | Reptiles | Primates | Rodents |
|---|---|---|---|---|---|---|---|---|
| Campylobacteriosis | X | X | X | X | X | |||
| Capnocytophaga canimorsus infection | X | X | ||||||
| Cat scratch disease (Bartonella henselae) | X | |||||||
| Leptospirosis | X | X | X | |||||
| Mycobacteriosis | X | X | ||||||
| Pasteurellosis | X | X | X | |||||
| Plague | X | X | X | X | ||||
| Psittacosis | X | |||||||
| Q fever (Coxiella burnetti) | X | |||||||
| Rat bite fever (Spirrillum minus, streptobacillus monliformis) | X | |||||||
| Salmonellosis | X | X | X | X | X | X | X | |
| Tularemia | X | X | X | |||||
| Yersiniosis | X | X | X | X |
Parasites
| Infectious Disease | Cats | Dogs | Fish | Birds | Rabbits | Reptiles | Primates | Rodents |
|---|---|---|---|---|---|---|---|---|
| Ancylostomiasis | X | X | X | |||||
| Cryptosporidiosis | X | |||||||
| Giardiasis | X | X | X | |||||
| Toxocariasis | X | X | X | |||||
| Toxoplasmosis | X | X | X |
Fungi
| Infectious Disease | Cats | Dogs | Fish | Birds | Rabbits | Reptiles | Primates | Rodents |
|---|---|---|---|---|---|---|---|---|
| Blastomycosis | X | |||||||
| Dermatophytosis | X | X | X | X |
The benefits of pet visits and animal therapy is well documented. Animals assist with emotional well-being and recovery from illness and injury. Animals in health care facilities under certain circumstances should be allowed and limited due to the risk of transmission of microorganisms to and from the animal. Zoonotic transmission includes viruses, bacteria, parasites, and fungi. It has been estimated that more than 6 out of every 10 known infectious diseases are spread from animals to people, and 3 out of every 4 new or emerging infectious diseases in humans are spread from animals. These diseases include Rabies, Plague, Salmonella and Influenza. Animals are at increased risk for acquiring diseases and becoming carriers of organisms while in the health care setting as a result of contact with patients, staff and visitors (reverse zoonoses). Dogs have been shown to be carriers of Methicillin-resistant Staphylococcus aureus (MRSA) and Clostridioides difficile (C. diff). Cats are known to transmit MRSA and toxoplasmosis.
Exotic animals and species identified as higher risk to cause human disease or injury should not enter the facility. These animals include but are not limited to: reptiles and amphibians (e.g., snakes, iguanas, lizards, turtles, frogs, salamanders), rodents (e.g., hamsters, gerbils, mice, rats), ferrets, raccoons, skunks, bats, nonhuman primates, hedgehogs, prairie dogs or other recently domesticated animal species
In respect for the health, safety and protection of the rights of residents, staff, visitors and other individuals providing care or services, the visitation of an animal should only be permitted under the following circumstances:
- Canine accompanying a uniformed on-duty law enforcement or security officer
- Service animals in accordance with the Americans with Disabilities Act
- Animal-Assisted Therapy
- Resident pet visitation.
Employee and visitor pets should be restricted from entering any part of the health care facility, including but not limited to hallways and offices. Only employees and visitors who participate in the Animal-Assisted Therapy Program or employees with service animals should be allowed in the facility.
All animals, including service animals, should not enter any area that meets the environmental criteria of restricted including:
- Sub-sterile environments
- Procedure areas
- Dialysis Areas
- Food preparation/consumption areas
- Medication preparation areas
- Clean supply rooms
- Other areas as designated by Infection Prevention and Control.
Animals should not visit residents who cannot perform strict hand hygiene, who have dermatologic conditions or who have barrier protective measures. This includes residents:
- On Isolation Precautions
- Who have uncontained wounds
- With Central Lines or Dialysis Catheters
- Who are on Reverse Isolation.
Animals should:
- Be up to date on their vaccinations, including rabies
- Have a health evaluation by a veterinarian in the last year
- Be well groomed (nails trimmed, not malodorous)
- Be bathed, if possible, prior to visiting
- Not eat raw meat within 90 days of visiting
- Be free of communicable diseases and parasites.
Animals should not visit at the onset or one week following:
- Episodes of diarrhea or vomiting
- Urinary or fecal incontinence
- Episodes of sneezing/coughing potentially related to an infectious agent
- The treatment with non-topical antimicrobials or any immunosuppressive medications.
Animals should not visit with:
- Open wounds or ear infections
- Skin infections or “hot spots”
- Conditions which might cause distress or pain to the animal
- A heat cycle.
Residents, staff and visitors should perform hand hygiene before and after touching an animal. This protects both the patient and the animal from harm.
Service Animals
- Employees should not exclude a service animal because they may be able to perform the same services that the service animal does
- Employees cannot exclude service animals because they perceive a lack of need for the service animal during the resident’s stay
- Inquire as to the purpose of the animal and document the purpose. DO NOT ask for the persons disability nor document the disability
- Are not required to wear identification
- Must be harnessed, leashed or tethered, unless these devices interfere with the service animal’s ability to work
- Only dogs are recognized as service animals under titles II (State and local government services) and title III (public accommodations and commercial facilities) the ADA
- Are working animals, not pets. They should not be touched or handled by any other residents, staff or visitors (unless assigned to do so).
Animal-Assisted Therapy
- All dogs and handlers that participate in the program should be certified in pet therapy by the Therapy Dog International or Pet Partners
- All therapy dog handlers are volunteers and should complete volunteer orientation
- Dogs should be watered using appropriate hand hygiene and care should be taken when handling the water bowl
- Any animal-assisted therapy visits should be documented in the resident’s medical chart.